12 Dec The Autoimmune Plague: Part III
Autoimmunity & Allergy: Two Sides of the Same Coin
 Paul A. Goldberg MPH, DC, DACBN, DCBCN
Paul A. Goldberg MPH, DC, DACBN, DCBCN
Consultant to The Goldberg Tener Clinic
Chronic Disease Reversal
Read Autoimmune Plague: Part I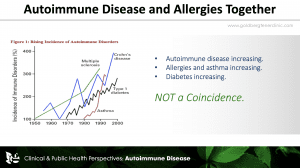
Read Autoimmune Plague: Part II
In Allopathic Medicine there are approximately ten thousand different “diseases” largely based on a patient’s symptoms. In the arena of autoimmune disorders alone there are one hundred forty different classifications all lacking a stated specific cause.
In assessing the cause(s) of autoimmune disorders, there is an intimate relationship between allergy and autoimmunity. This important connection is poorly understood and has largely gone unrecognized by the medical community.
Autoimmune disorders, seasonal allergies, asthma, and food allergies have dramatically increased in their prevalence and severity in our nation. A literature search, however, rarely shows medical physicians taking note of this association. I located only one study prior to 2018, reported in Acta Medica Scandinavia in 1955, that looked at the relationship of Inhalant Allergies and any type of Autoimmune Disease, in this case ulcerative colitis.[i] Even now there is only scant attention given to this phenomenon. If we look at public health studies, inhalant allergies, food allergies and autoimmune disease have sharply increased simultaneously over the past half century.
Recently, as reported in The European Respiratory Journal, the long-term risk of autoimmune disorders was found to be significantly higher in patients with allergic diseases. Allergic diseases and autoimmune disorders co-occur frequently.[ii]
This is important in addressing the causes of autoimmune disorders and improving a patient’s health. The basis of allergy is the concept of self vs. non-self, i.e., that an allergy occurs when the body over-reacts to materials that are foreign to it. The basis of autoimmune disease is when the body over-reacts, for some reason, to its own tissues i.e., to self. In both allergy and autoimmunity there is an over-reaction of the immune system. To see these as separate entities is an error. Autoimmunity and allergy are simply two sides of the same coin and not so different from each other. It is therefore not difficult to understand why the child with severe allergies is more likely to be the adult with autoimmune disease. The patient interview shown below with a young man from our clinic that recovered from Juvenile Rheumatoid Arthritis and severe allergies illustrates this connection.
Indeed, we often hear from patients who have Rheumatoid Arthritis, Inflammatory Bowel Disease, Psoriatic Arthritis, Psoriasis, Ankylosing Spondylitis or other autoimmune related issue that they “used to have allergies but they outgrew them”. What we frequently point out to them is that they did not so much “outgrow” their hay fever or asthma or severe food allergies but rather experienced a change in the way their body expressed itself, i.e., from allergy to autoimmunity.
To add to this allergy/autoimmune relationship, in both instances histamine, produced by the mast cells, is a key player. Most people identify allergies with histamine but histamine is also a major player in autoimmune processes. Excessive histamine results not only in the typical sneezing and runny nose as found in hay fever and asthma but also can result in inflammatory reactions in the joints, muscles, gastrointestinal tract and other body tissues as seen in inflammatory bowel disease, R.A., A.S. and other autoimmune disorders. Patients with these issues often report an exacerbation of their symptoms in the Spring and Fall when the pollens are highest.
Osteoarthritis can also represent a long term allergic/autoimmune component exhibiting excessive histamine release by mast cells in the joints, resulting in cartilage degeneration over time. Scientists at Stanford University have linked mast cell activity to the development of osteoarthritis.[iii] Mast cells produce a degradative protein, tryptase, that can damage collagen and other molecules that form the cartilage in joints. Osteoarthritis should also be considered, at least in part, as an allergic/autoimmune related disorder.
Of Special Note:
- Inflammatory cytokines such as Tumor Necrosis Factor Alpha are well associated with autoimmune disorders such as R.A., A.S., P.A. and Inflammatory Bowel Disease and are also produced by mast cells, the same cells that produce histamine.
- Elevated levels of IgE associated with allergy are commonly found in autoimmune disorders and autoimmune disorders tend to worsen as IgE increases.
- The rapid rise in autoimmunity in the U.S. population is paralleled by a rapid rise in allergies in both adults and children.
As I have discussed in previous newsletters, it is important to identify causal factors in every patient with autoimmune Disease. The Medical Approach does not seek out causal factors and their treatments carry significant risks (see articles “The Problems with Prednisone” and “The Dangers of Biologicals“).
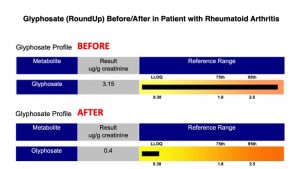
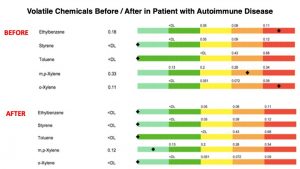
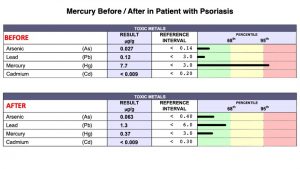
In addition to allergic connections, other factors we commonly find in our patients with autoimmune illness include exposure to an ever-increasing amount of toxins in our environment affecting people in all walks of our society. This includes toxic materials from air, water, food, home building materials, industrial, pharmaceutical, occupational and related sources. A bodily burden never before experienced in human history is occurring. Some of the more recognized toxins found in human tissues that may contribute to autoimmune illness include arsenic, atrazine, dioxins, lead, mercury, perfluoroalkyl substances (PFAs), asbestos, BPA, phthalates, radon, VOCs, RoundUp (Glyphosate), pesticides, herbicides, organophosphates, noxious gases, particulate matters along with a wide array of plastic related materials. Using clinical epidemiology, toxicological evaluation and nutritional chemistry we are able to identify these issues and guide the patient in how to address the particular issues we identify. Shown below are a few examples of before/after toxicology studies conducted on patients at our clinic that came to see us with autoimmune / allergic related disorders. Testing procedures conducted at the Goldberg Tener Clinic allow us to measure/quantify body accumulation of over two hundred toxic environmental compounds.
GI Malfunction/Nutritional Biochemistry issues are another factor. These types of issues result from unhealthy diets, poor eating habits e.g., overeating / eating under stress and repeated use of antibiotics and other drugs, all resulting in disturbances in the microbiome and immune responses.
Long term emotional stressors from family life, work and other sources also can play a contributing role and we make an effort to identify these as well and bring them to our patients’ attention.
These and other causal factors stimulate and overburden the immune system causing it to become overactive. This can result in “friendly fire” where the immune system is so overwhelmed that it attacks our own tissues in an attempt to protect our body from what it sees as negative “non-self” outside forces.
Autoimmune Disease is rapidly increasing. It destroys lives. By doing a detailed evaluation of each patient we have been able to stop and reverse the autoimmune process in the majority of our patients…not by treating the condition but by identifying and addressing causal factors that have contributed to the patient’s impaired health. The before/after pictures shown below illustrate the good outcomes that are possible. Click here to see interviews with patients from our clinic that regained their health from autoimmune / allergic disorders.




Related Articles by the Goldberg Tener Clinic
1) Reversing Autoimmune Disorders
2) Reversing Chronic Skin Conditions
3) An Effective, Causal Based Approach to Digestive Problems
4) Reversing Rheumatoid Arthritis and other Rheumatoid Conditions
5) Reversing Thyroid Conditions
6) Small Intestinal Bacterial Overgrowth (SIBO): A Symptom of Impaired Health
7) Irritable Bowel Syndrome: A Meaningless Diagnosis
8) The Facade of Functional and Alternative Medicine
9) An Effective, Comprehensive Approach to Reversing Allergies
10) You have been misled… the way to lose weight is NOT trying to lose weight.
11) Click here to see our full library of articles.
REFERENCES
[1] Acta Medica Scandinavia. Vol. CLII, Pasc. II, 1955. Chronic Ulcerative Colitis Due to Pollen Allergy with Six Case Reports.ALBERT H. ROWE, M. D., ALBERT ROWE, Jr., M. D. and KAHN UYEYAMA, M. D.
[2] European Respiratory Journal Allergic diseases and long-term risk of autoimmune disorders: longitudinal cohort study and cluster analysis Mamidipudi Thirumala Krishna, Anuradhaa Subramanian, Nicola J. Adderley, Dawit T. Zemedikun, Georgios V. Gkoutos, Krishnarajah Nirantharakumar2019 54: 1900476; DOI: 10.1183/13993003.00476-2019 http://bit.ly/33tqkZn
[3] https://med.stanford.edu/news/all-news/2019/05/mast-cells-crucial-to-causing-osteoarthritis.htmla




No Comments