18 Sep A Nation on Statins

Millions of Americans are on drugs and diets that may miss the mark and ignore the causal factors involved with Cardiovascular Disease

Paul A. Goldberg MPH, DC, DACBN, DCBCN
Consultant to The Goldberg Tener Clinic
Chronic Disease Reversal
A version of this article will be published in the upcoming Georgia Chiropractic Association Fall Magazine.
Statin drugs are the number one prescribed pharmaceutical in the United States. Physicians place millions of Americans on them based on their elevated LDL cholesterol levels which supposedly place them at a significantly increased risk of Cardiovascular Disease.
Statins are cholesterol-lowering drugs. They are the most common class of lipid-lowering medications employed to reduce LDL cholesterol levels. Their usage is based on the hypothesis that CVD (heart attack and stroke) are the outcome of elevated LDL Cholesterol and that by lowering LDL levels, a patient’s risk of CVD will be lowered.
Public Health Data
- Cardiovascular Disease (CVD) or coronary heart disease (CHD) is the leading cause of death in the United States, accounting for 928,741 deaths in the year 2020.
- Between 2018 and 2019, direct and indirect costs of total CVD were $407.3 billion ($251.4 billion in direct costs and $155.9 billion in lost productivity/mortality).
- In 2020, coronary heart disease (CHD) was the leading cause (41.2%) of deaths attributable to CVD in the United States, followed by stroke (17.3%), other CVD (16.8%), high blood pressure (12.9%), heart failure (9.2%) and diseases of the arteries (2.6%).[1]
Patients with Cardiovascular Disease are known to have a buildup of plaque, largely comprised of cholesterol in their blood vessels. In the 1970’s and 1980’s, there was an aggressive movement indicting the consumption of saturated fats / cholesterol as being responsible for the preponderance of Cardiovascular Disease in the United States. This was influenced by the work of Ancel Keys and Harvard University Nutrition Professors. The assumption has been that cholesterol containing foods/saturated fats are the major players in the etiology/evolution of CVD. This has led to the development and widespread application of Statin Drugs to address CVD.
Have we come to the right conclusion about the cause(s) of CVD and is the massive medication of the U.S. Public with Statin Drugs the appropriate solution? This is an important multifaceted public health topic to which this article will serve as an introduction.
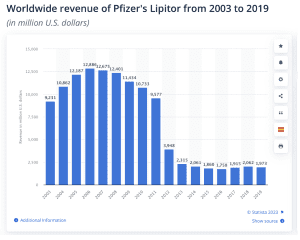
Statins are the most widely prescribed cholesterol-lowering drugs in the world. [1] Despite the expiration of their patents, revenue continues to rise with total sales estimated at over a trillion dollars per year. There are many concerns that the benefits of Statins have been exaggerated, the risks have been underplayed and the fundamental basis on why the drugs have been employed highly faulty.
Background:
German pathologist Rudolf Virchow (1821 – 1902) observed that the artery walls of patients dying of occlusive vascular disease contained a yellowish fatty substance termed atheroma, the Greek word for porridge, and identified as cholesterol. Anitschkow and Chalatow in 1913 showed that feeding cholesterol to rabbits (who do not ingest cholesterol containing foods in their natural diets) rapidly produces atheromatous disease like that found in man.
The Framingham study in the 1950’s prospectively studied the relationship between blood cholesterol and other potential risk factors and death from CVD and showed a correlation between high plasma cholesterol and CVD mortality.
The major event leading to the hypothesis that elevated LDL Cholesterol levels were responsible for CVD came out of the work of Physiologist Ancel Keys (1904 – 2004) who focused on the relationship between diet and disease. He launched the Seven Countries Study in 1958 after exploratory research on the relationship between dietary patterns and the prevalence of coronary heart disease in Greece, Italy, Spain, South Africa, Japan and Finland showed that northern European countries and the United States had both high plasma cholesterol and high CVD mortality rates. Plasma cholesterol and CVD mortality were substantially lower in southern Europe and even more so in Japan.
Keys contended that the association with CVD mortality was attributable largely to low-density lipoprotein (LDL) cholesterol. This led to the hypothesis that elevated LDL cholesterol was causally related to coronary disease and that reducing it would lower the risk of coronary events. This hypothesis led to the popularity of diets low in saturated fats and cholesterol and a push for the development of drugs that could be taken to lower cholesterol levels in the body… the chief among them are “Statin Drugs’.
Ancel’s work was reinforced by studies at Harvard University School of Public Health by Frederick Stare and Mark Hegsted who worked with a trade group called the Sugar Research Foundation, which was trying to influence public understanding of sugar’s role in disease, i.e., that sugar did not play a role. The trade group solicited Mark Hegsted, Frederick Stare and Dr. Robert McGandy, professors of nutrition at Harvard, to write a literature review aimed at countering early research linking sucrose to coronary heart disease. The group paid the equivalent of $48,000 in 2016 dollars to Hegsted, McGandy and Stare.
The Food and Beverage industry thus directed attention away from the potential role of sugar/carbohydrates in the diet and pointed blame at saturated fats and cholesterol as being the primary etiological factors in CVD.
The National Institutes of Health (NIH) Coronary Primary Prevention Trial (USA), an NIH Consensus Conference, convened in 1984 and concluded that lowering elevated LDL cholesterol with diet and drugs would reduce the risk of CHD. The NIH accepted the findings of the Consensus Conference and the following year initiated a program to educate physicians and the public about the importance of treating hypercholesterolemia.
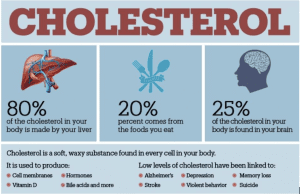
We should recognize in exploring this topic that cholesterol is critical to the human body forming the backbone of hormones among other functions.[1]
In the rabbit, monkey and dog, the drug Compactin was shown to lower plasma cholesterol. In 1978, Alberts, Chen and others at Merck Research Laboratories found an inhibitor of HMG-CoA and named their discovery officially as lovastatin. This was the beginning of the widespread use of prescription statin drugs.
Statins work in two ways to reduce cholesterol:
- Limiting the production of cholesterol by the Liver by blocking the enzyme that creates cholesterol.
- Reabsorbing existing cholesterol.
How much do statin drugs lower CVD risk? Much of this depends on whether we are looking at an absolute risk reduction or a relative risk reduction.
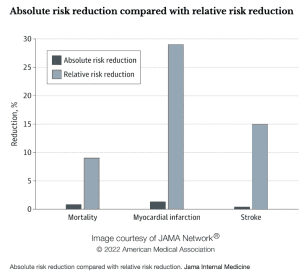
Imagine your chance of dying from a certain condition prematurely is 0.2%, and there’s a drug that reduces your chance of dying to 0.1%. In relative terms (relative risk reduction), your chance of dying has been halved, or reduced by 50%. But in absolute terms (absolute risk reduction), your chance of dying has only gone down by 0.1%.
Absolute risk reduction presents a clearer picture and makes it easier for people to make informed decisions.
In a study published in Jama Internal Medicine [1], the absolute risk reduction from taking statins was modest compared with the relative risk reduction. The relative risk reduction for those taking statins compared with those who did not was 9% for deaths, 29% for heart attacks and 14% for strokes. Yet the absolute risk reduction of dying, having a heart attack or stroke was 0.8%, 1.3% and 0.4% respectively.
Statin Side Effects
In animals, statins produce significant toxicity at high doses, increases in hepatic transaminases, atypical focal hyperplasia of the liver, vascular lesions in the central nervous system (CNS), skeletal muscle toxicity, testicular degeneration and tumors of the liver and other sites. Supposedly these side effects have not been demonstrated in human trials.
In 2010, the British Medical Journal published a study that statins may raise cataract and kidney risk. Researchers estimated that for every 10,000 people taking a statin, there were about 271 fewer cases of heart disease, 8 fewer cases of esophageal cancer, 307 extra patients with cataracts, 23 additional patients with acute kidney failure, and 74 extra patients with liver dysfunction.
On March 3, 2012, the FDA announced changes to the safety information on the labels of statins: there is an increased risk of higher blood sugar levels and of being diagnosed with type 2 diabetes. In addition, the statin labels will also now reflect reports of certain cognitive effects such as memory loss and confusion experienced by some patients taking the drugs.
Statin induced muscle disease. Muscle complaints are common in statin users, occurring in more than 10% of this population. Myalgia or muscle pain occurs in about 7% of statin users.
Rhabdomyolysis: Some people who take statin medications to lower their cholesterol may have severe muscle pain, a symptom of rhabdomyolysis. This a serious condition that causes muscle cells to break down.
The Elephant In The Room
For decades, mainstream medicine has spent millions of dollars in perpetuating the idea that high cholesterol is the cause of CVD. As a result, millions of Americans (1 in 4) are now taking a statin drug. There is, however, increasing evidence to suggest that these drugs have a dark side to them and are based largely on a faulty hypothesis that elevated LDL cholesterol is the cause of cardiovascular disease. This appears to be based on more of an association rather than a causal relationship. In the following video, “Heart of the Matter: The Cholesterol Drug War“, ABC News investigates the science behind the claims that high cholesterol causes heart disease and explores the dark side of statin drugs.
The dangers associated with statin drugs are well established, with numerous studies showing adverse effects include muscle problems, anemia, increased cancer risk, diabetes, kidney and liver damage, cataracts and sexual dysfunction.
Conflicting Schools of Thought
A conflicting school of thought is that CVD is related to the intake of sugar/excessive carbohydrates.
Around the same period in 1958 when Ancel Keys was asserting that fat was to blame for the rise in heart disease, British physiologist John Yudkin found that sugar appeared to correlate with heart disease in several countries and put forth his competing hypothesis that high sugar consumption was a key cause of heart disease.
Unlike Yudkin, Keys was unwavering in his belief that the escalation of heart disease was being fueled by saturated fat. In response, Yudkin took to the Lancet to accuse Keys and his colleagues of using ‘awkward facts’ and ‘cherry-picking only the data which supported their view’.[5]
The debate continues. Saturated Fat? Cholesterol? Sugar/excessive carbs? The stakes are high. Epidemiological studies of native peoples such as the Maasai, a Nilotic ethnic group inhabiting southern Kenya and Northern Tanzania, do not support a high cholesterol intake as being a primary factor in CVD.
The evidence is also clear that initial studies implicating LDL Cholesterol were highly biased and that the focus on CVD being caused by elevated LDL Cholesterol is supported by a trillion-dollar statin drug industry advocating a group of drugs that pose two significant dangers… missing the mark in terms of addressing etiological factors and having a long list of hazardous side effects.
Evaluating and Addressing Cardiovascular Disease Risk
Cardiovascular Disease is a complex issue involving a variety of factors. The medical emphasis on cholesterol as a primary contributor and subsequent treatment with statin drugs has reduced attention on other important etiological factors needing to be carefully identified and addressed in each case. A proper assessment, as performed at the Goldberg Tener Clinic, starts with a detailed history exploring family history / genetics, lifestyle, diet / nutrition, drug and surgical history and stress factors followed by a physical exam. Comprehensive laboratory studies evaluating a variety of risk factors (not just cholesterol) including HsCRP, Oxidized LDL, blood sugar metabolism, fatty acid balance, toxicology and others is essential to understanding each patient’s risk and developing an individualized Bio-Hygienic program to lower that risk.
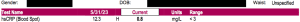
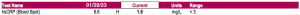
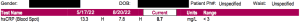
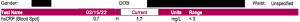
One of the best blood indicators for assessing risk for Cardiovascular Disease is the High Sensitivity C-Reactive Protein test. It is one of several markers that can be employed as a pre-post measure to monitor patient progress and ensure a successful reduction in Cardiovascular Disease risk.
The following are before/after HsCRP test results from patients at the Goldberg Tener Clinic evaluated to be at high risk for cardiovascular disease. The improvements came by addressing causal factors and without the use of drugs, herbs or other treatments/therapies. Learn more about our unique approach to Chronic Disease Reversal, the Bio-Hygienic Re-Creation System™.
Click here to see video interviews with patients at the Goldberg Tener Clinic that came to see us with Cardiovascular Disease.
High Risk: Greater than 3.
Normal: Less than 3.
Ideal: Less than 1
[1] https://professional.heart.org/en/science-news/heart-disease-and-stroke-statistics-2023-update
[2] https://pubmed.ncbi.nlm.nih.gov/29353811/
[3] https://www.doctorkiltz.com
[4] https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2790055
[5] Yudkin, Diet and Coronary Thrombosis, 162.




No Comments